Preexisting immune response to SARS-CoV-2
https://science.sciencemag.org/content/370/6512/89.full
Robust T cell responses to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus occur in most individuals with coronavirus disease 2019 (COVID-19). Several studies have reported that some people who have not been exposed to SARS-CoV-2 have preexisting reactivity to SARS-CoV-2 sequences. The immunological mechanisms underlying this preexisting reactivity are not clear, but previous exposure to widely circulating common cold coronaviruses might be involved. Mateus et al. found that the preexisting reactivity against SARS-CoV-2 comes from memory T cells and that cross-reactive T cells can specifically recognize a SARS-CoV-2 epitope as well as the homologous epitope from a common cold coronavirus. These findings underline the importance of determining the impacts of preexisting immune memory in COVID-19 disease severity.
Category: Science
AAPS considers the possibility of a ‘casedemic’
Latest in a growing list of sceptics with regards to “a second wave of Covid” is the Association of American Physicians and Surgeons, which says:
Will the huge rollout of COVID tests help end the pandemic—or assure that it will never end?
We have had pseudo-epidemics before. In 2006, much of Dartmouth-Hitchcock Medical Center was shut down, and 1,000 employees were furloughed or quarantined, because whooping cough was thought to be spreading like wildfire based on 142 positive PCR tests.
The employees also had cultures taken, and a couple weeks later not a single one had a positive culture for the slow-growing bacteria, Bordetella pertussis. There had simply been an outbreak of some other ordinary respiratory disease, not the dreaded whooping cough. Gina Kolata wrote in The New York Times: “Faith in Quick Test Leads to Epidemic That Wasn’t.”
It is not so easy to culture a virus, and cultures of SARS-CoV-2 are not routinely done. Unlike in previous epidemics (SARS-CoV-1, H1N1 influenza, Ebola, or Zika), World Health Organization (WHO) guidance has no requirement or recommendation for a confirmatory test in COVID-19.
There is surprisingly little information on the false positive rate of PCR tests for COVID. That all lab tests have false positives should not be controversial, but this idea “has been entirely rejected by governments and the medical establishment, writes Mike Hearn.
For all tests, the predictive value of a positive test depends on the prevalence of disease. If most of the persons tested are free of disease, a positive test may be more likely to be a false than a true positive. This could at least partially explain the reports of large numbers of asymptomatic carriers of SARS-CoV-2.
Failure to recognize the problem of false positives has consequences—such as possible quarantining of uninfected with infected individuals.
The dreaded “second wave” might be a surge of false positive tests that are inevitable in mass screenings of healthy persons.
If you get a positive PCR result, you might want to get a confirmatory test, for example antibodies, especially if you are not sick. Positive or not, you might want to be sure you have adequate levels of vitamin D and zinc, and access to a physician willing to prescribe early home treatment.
For more information:
“What Does a Positive PCR Test Mean?”
“COVID-19 Statistics and Facts: Meaningful or a Means of Manipulation?”
Coronaviruses: how they spread, how to protect oneself, and more
This great article in Dutch is an interview with doctor, epidemiologist and professor emeritus Menno Jan Bouma. Below, I am going to copy and paste a Google-generated English translation which is very intelligibile.
However, before that, I am going to summarise what he says about how viruses such as coronaviruses actually spread:
- They spread through droplets; they leave a host in droplets and still wrapped up in these droplets they need to reach the new host.
- The smallest of these droplets are called aerosol. These are the most dangerous because, unlike heavier droplets which fall on the ground within seconds, the aerosols can remain suspended in air for longer, and thus they can be breathed in by people.
- The virus really becomes dangerous if it reaches the lungs, where the immune system is the weakest.
- If the virus reaches mouth and nose in a bigger droplet (non-aerosol), the overwhelming majority of times it will get stopped by the immune system defences present in nose and throat.
- If the virus reaches mouth and nose in aerosols, there are far greater chances to get straight through to the lungs.
- Coronaviruses are seasonal and thrive in cool, dry air. In these conditions, aerosol circulate for much longer.
- Because of the above, enclosed non-ventilated spaces are the most likely places where one can get infected.
- Ventilation and humidity are important, and most likely to get rid of any traces of the virus.
Then some recommendations:
- Keep your immune system in good shape; take extra doses of Vitamin C and D; take also Vitamin P (euphemism for pleasure, that is, take care of your psychological state, meet with friends, have fun, stay psychologically healthy)
- Avoid super-spread events, that is, avoid staying long hours with people indoor in a poorly ventilated space
Then final question: what about washing hands, sanitising and social distancing/no touching?
- Those measures are perfect for tackling viruses such as diarrhoea viruses. These viruses travel from host to host through hands, through surfaces, and through touch. Indeed, if you want to deal with these viruses, it is very good to disinfect everything and to keep your distance and not touch each other.
- But now we know that coronaviruses have a different strategy of traveling from host to host, and of invading hosts. They mainly spread by air. Compare it with cigarette smoke: it hardly spreads through hands or surfaces. Try comparing this to blowing cigarette smoke on your hands, and then give another one a hand or a hug. The chance that your cigarette smoke will end up deep in the lungs of the other person in this way is minimal. Coronaviruses need a lift of aerosols in order to get deep into the lungs where our body has less resistance. The measures washing hands, disinfecting, keeping your distance, no shaking hands and no cuddling are therefore not or hardly effective when you want to tackle viruses such as flu viruses or coronaviruses.
Full article in English
Doctor, epidemiologist and professor emeritus Menno Jan Bouma lived in Oost for years. As a guest lecturer he gave lectures at the Tropical Institute in East. He now lives in Ireland, but still likes to come to the East on a regular basis. He devoted his life to researching the ecology and distribution of viruses and other pathogens. In this time of the coronavirus, I would like to know a little more about viruses. So that’s what I’m talking to him about.
Interview | Ruby Tilanus
You worked at the Tropical Institute in London, but came back to teach at our Tropical Institute in East. How was that?
Awesome. There are only a few places in the world with an enormous amount of knowledge about infectious diseases. The Royal Tropical Institute in East was one of them. Unfortunately, in the 1960s, many thought we had mastered infectious diseases, and in and after the 1980s, the Tropical Institute was largely cut back. The library has been closed. Specialists, collections and books disappeared. Much knowledge has thus been lost. And where knowledge is lacking, fear lurks.
That knowledge could now have come in handy in tackling the corona virus.
Indeed.
Fortunately, you are still here and you want to share your knowledge about viruses with us. First of all, tell us what is a virus anyway?
A virus is not a “living” being like you and I are. A virus is not ‘alive’.
A virus consists of genetic material (DNA or RNA) surrounded by a packaging (a shell). A virus cannot do anything without a ‘host’ or ‘hostess’. It’s as dead as a piece of plastic. It doesn’t show any sign of life.
But if a virus is lucky enough to enter cells in a host’s body, it will behave like a hibernating bear.
The virus uses its host’s nutrients to reproduce itself. That is the only thing a virus can do and a piece of plastic cannot. That is the only thing that a virus itself, actively, can: reproduce itself. Although: itself, active… for this a virus does need a host.
What happens to a virus after it reproduces?
After reproducing, the new young viruses start looking for a new host.
That is where such a young virus has to travel to and penetrate. That is quite difficult for the virus, since it cannot do anything on its own, except reproduce itself. He has to travel passively or hitch a ride, and then try to penetrate somewhere. If that is successful, the virus feast of reproduction can take place again. So the virus cycle is: travel, invade, reproduce itself, travel, invade, reproduce itself and so on. A virus cannot or does not do anything else. Because a virus is not ‘alive’.
How do viruses do that: passive travel and passive entry? A virus has no wings, no legs and no webbed feet to travel, does it? And a virus cannot just enter through your skin, can it?
Right! A virus has no wings, no legs, and no webbed feet to travel from one host to another. And indeed, a virus cannot just enter through your skin. Your skin is literally an impenetrable barrier to a virus.
Viruses have evolved various strategies to travel and invade their hosts. The way a virus travels is directly related to the way the virus enters the body of its host after its journey. So you always have a way of traveling and a way of penetration that are linked to each other. Each virus type specializes in at least one of those strategies. On that basis, you can divide all viruses out there into roughly three different main groups.
Please tell me a little more about those different main groups of viruses…!
You can give the main groups the following names:
– ‘Opportunists’: they enter the body through damage such as a wound or a blood transfusion (think of the AIDS virus);
– ‘Survivors’: they follow the path of food (think of diarrhea viruses);
– ‘Kites’: they hitch a ride with the air that is inhaled (think of flu viruses and corona).
First you mention: Opportunists (such as the AIDS virus). What is the strategy of Opportunists?
An opportunist waits until he finds an opening somewhere in the skin of the new host, a wound for example. Then he waits until his old host makes direct contact with that wound with his blood or with his semen. And then it enters the body of the new host through that wound. Opportunists can also enter via an insect sting (sting).
And Survivors (such as diarrhea viruses)? What is their strategy?
Survivors can withstand the extreme acidic gastric juices and the extreme conditions of the intestines, and can survive there. They reproduce in the intestines. If an old host does not wash his hands after defecating, a tiny amount of feces can get on the hands of the old host, which can then end up on a table, elevator button, or other surface, for example. If the new host touches that surface, or shakes hands with the old host, the Survivor may end up on the hands of the new host. If the new host then licks his fingers and does not wash his hands before eating, the Survivor can pass through the mouth into the stomach and intestines of the new host.
What interests me especially in this time of corona: what is the strategy of Vliegers (such as influenza viruses and corona)?
The strategy of kites is to hitch a ride with small droplets that the old host lets out through the mouth. When the old host exhales, talks, sings or coughs, small droplets come out of his mouth. Kites try to hitch a ride with those little droplets. A lucky kite will leave the body of the old host in a tiny droplet. It then travels through the air to a new host and enters the body along with the inhaled air. There he tries – still packed in a drop – to hitchhike up to the alveoli, deep in the lungs. Deep in the lungs, the lung wall is very thin: only one cell layer thick. Our immune system is weak there: far fewer virus particles are needed to make you sick.
How small are those droplets really?
The droplets are all small. But some droplets are many times smaller than other droplets. We call the smallest droplets ‘aerosols’ and they can fly.
The larger droplets do not float in the air for long. They fall to the ground within seconds due to gravity. They cover a distance of about half a meter with normal breathing to a few meters with a strong cough. To reach the new host, the Flyers must get to the nose or mouth level of the new host. However, the larger droplets soon bend towards Earth due to gravity. The aerosols remain floating in the air for a very long time. If not properly ventilated, they can continue to circulate in the air for hours. They can cover enormous distances.
Okay, this is the story on the part of the viruses. But what about our side of the story? What is our defense against viruses?
Man has been living with viruses since its inception. We and our distant ancestors in the animal kingdom evolved along with the viruses, as it were. There are many forms of innate and acquired defenses that have developed over time. Antibodies are just one of them. We have developed appropriate defense strategies for each of the different strategies of viruses for survival (Opportunists, Survivors and Airmen).
Tell us: what is our defense strategy against Opportunists (such as the AIDS virus)?
Our oldest defenses may have been developed against Opportunists. We have skin. Our skin blocks almost everything harmful that our body wants to enter. When we have a wound, our body is very well able to heal that wound very quickly.
And what is our defense strategy against Survivors (such as diarrhea viruses)?
We have developed a very sour stomach for them. Our gastric juice damages almost all viruses, so that they can no longer reproduce. Most Survivors also do not survive our gastric juice – only the few who do get the chance to reproduce.
And now the most important thing: what about our defenses against Kites (such as flu viruses and corona)?
To get deep into the lungs, a Kite must first pass through the mouth or nose. We all have multiple defense mechanisms in our nose, mouth and throat, including immune cells. An entire army with a vanguard, a rearguard and many layers of commanders is ready to stop the Flyers.
Most intruders get stuck in the labyrinth of mucous membranes and small hairs in your nose and are defused here. The mouth and pharynx also participate in the defense against the Airmen. If they get into the stomach, they don’t stand a chance there.
Does it matter whether a Kite enters through a large or a small drop (aerosol)?
Yes. If a Kite hitches a ride with a small drop (aerosol), the chance of breaking right through the defense line is much greater than with a large drop. Just as small fish are much more likely to slip through the mesh of a net than large fish. Together with the inhaled air, the Vlieger can also – if he is lucky – fly deep into the lungs. After all, the drop is so small that – with a bit of luck – it can go straight into the lungs. The Vlieger virus then hitches a ride with the aerosol.
When a Kite hitches a ride in a big drop, he has a much harder time at the entry of the new host. The chance that he will be stopped at the port (in the nose, mouth or throat) is then maximum.
What exactly happens in the nose?
Everything in the nose is designed to prevent viruses, bacteria and other germs from entering our body. In addition to the nose, the mouth and throat are also extremely adept at this. Our defenses are ready to deal with intruders. In most cases we manage to effectively stop intruders (such as viruses and bacteria) in the nose and make them harmless. In the meantime, we have ‘become acquainted’ with the intruder. This means that the next time the same intruder shows up at our front door again, we can intervene all the faster and more effectively. You can compare that to a kind of standing up and getting acquainted at the front door: our body becomes acquainted with the previously unknown virus, and can start to build up resistance and make antibodies against the virus.
You have researched the role of the seasons and the weather on the spread of infectious diseases. Does that also play a role in the spread of corona?
Yes, most infectious diseases are seasonal diseases. For Vliegers, this mainly has to do with the temperature and the humidity. Kites such as flu viruses and corona thrive in cool, dry air, while Survivors dry out faster and die in dry air. It is not yet entirely clear whether the humidity is bad for the virus itself or for the life of the aerosol. In moist air, aerosols may quickly deflect to the earth. In dry air, aerosols can keep circulating for much longer. In the summer we have seen many cases of corona in the meat processing industry: there the air is kept cool and dry and in order to save costs, the outside air is insufficiently refreshed: a ‘mecca’ for Vliegers (aerosols). In winter we heat our houses and we are more indoors.The air dries out and we live together in a smaller space. You can then ingest a larger dose of viruses into the lungs, your most vulnerable place. That makes flu and corona real winter viruses. Savings on heating (from draft excluders to intelligent systems that only supply fresh air when it is really needed) is usually at the expense of fresh and more humid outdoor air. So we have to be careful with that!
With the winter season approaching, I advise everyone to ensure good humidity in the house. By putting a bowl of water on several radiators, for example.
Do you think it is wise to meet up with people outside?
Meeting outside is indeed sensible. You can compare the behavior of aerosols with the behavior of cigarette smoke. If you smoke a cigarette outside, your smoke will dissipate quickly and will not bother others except when you blow them in the face. It is the same with aerosols. If you carry the corona virus and you meet up with people outside, they will not be bothered by your aerosols. Except when you blow them in the face.
And what about ventilation exactly? Does that make sense?
Yes, that certainly makes sense. Compare it again with cigarette smoke. If you go to smoke a cigarette in my living room and I don’t ventilate properly, well, I can still smell your cigarette later on. But if I open the windows opposite each other for a while, the smell will disappear in no time.
It is the same with aerosols. If you ventilate well and open the windows together, they are gone in no time. Especially in winter, the peak season for the virus, fresh outside air is very important.
What more can we do to contain Kites such as the corona virus?
Very important in the fight against all infectious diseases is: ensure that your natural defense system can function properly. Think of a healthy diet, sufficient exercise and enough sleep. Take an extra dose of vitamins C and D daily for strengthening: these vitamins help your immune system.
Also ensure psychological well-being. We call this ‘vitamin P’ where the P stands for pleasure. Do things that make you happy. Dance, make music, meet friends, go out.
And always avoid super spread events.
What do you mean super spread events? Tell me more about it…
The coronavirus can spread super fast during so-called ‘super spread events’. These are events where many people spend hours together in a poorly ventilated space. Think, for example, of Après-ski bars or carnival cafés. Only one person needs to carry the corona virus. That one person unnoticeably blows many aerosols into the air. Probably some coronavirus carriers do this more intensely than others. All those present then inhale these aerosols for hours. The virus has a very good chance of invading many, in numbers that our defenses cannot handle.
I don’t hear you about washing hands, disinfecting, keeping your distance, not shaking hands, and not hugging…!
Those measures are perfect for tackling Survivors such as diarrhea viruses. Survivors travel from host to host through hands, through surfaces, and through touch. Indeed, if you want to deal with these viruses, it is very good to disinfect everything and to keep your distance and not touch each other.
But now we know that corona is a Kite. Kites have a different strategy of traveling from host to host, and of invading hosts.
As said: Kites mainly spread by air. Compare it again with cigarette smoke: it hardly spreads through hands or surfaces. Try blowing cigarette smoke on your hands, and then give another one a hand or a hug. The chance that your cigarette smoke will end up deep in the lungs of the other person in this way is minimal. Kites need a lift of aerosols in order to get deep into the lungs where our body has less resistance. The measures washing hands, disinfecting, keeping your distance, no shaking hands and no cuddling are therefore not or hardly effective when you want to tackle Kites such as flu viruses or corona.
But Menno, isn’t that diametrically opposed to what Mark Rutte asks of us ?!
Partly yes. But Rutte has also asked us several times to use our common sense …
I’ve heard you say, “Viruses are like burglars. You have to stop them at the front door. ‘ What exactly do you mean by that?
There is a big difference between a burglar who is stopped at the front door, and a burglar who enters your house for a moment and then walks out, and a burglar who is going to settle in your house and live there. It is the same with viruses. If you ‘stop a virus at the front door’, that is, if you stop a virus in your nose, mouth and throat and make it harmless, then you are doing well. You will literally get to know the virus up close, so that you can react even faster next time. If you briefly inhale a virus and then exhale it again, there is not much going on either. But if a virus settles deep in your lungs and starts to reproduce there, yes, it can make you very sick.
We are currently seeing a huge increase in the number of corona infections. Also here in East. How do you feel about that?
The infections are now measured with the so-called ‘PCR test’. This test examines whether you have the coronavirus in your nose, mouth or throat, or leftovers of the dead virus if the infection has already passed. Many people who have the virus in their nose, mouth or pharynx are busy ‘getting acquainted and standing by the front door’. As I just said: in normally healthy people with a normal immune system, there is a whole army of immune cells ready in your nose, mouth and throat. That army is introduced to the virus, makes the virus harmless, and at the same time has gotten to know the virus and so it can react even better next time. I personally think that the word ‘contamination’ is therefore not so well chosen. I would rather speak of ‘acquaintance’. Yes,it is true that the number of ‘acquaintances’ with the virus is increasing (enormously).
But isn’t it really bad that the virus is in the nose of more and more people?
Yes and no. People who have come to know the virus and have managed to survive at the front door function as a kind of ‘living shield’ for all the vulnerable in our society. I am talking here about the famous ‘group immunity’. As a community you need some time to build up group immunity. Young, vital people generally have little or no problems with corona. It almost always remains with them sniffling a little. In the Netherlands there is a great sense of togetherness, and the care for the elderly is wonderful. A nice matching slogan could be: “Take care of your grandmother: make sure you have had corona.” The more young, vital people have become acquainted with the corona virus and have kept the virus standing at the front door, in other words: have become immune to corona,the more favorable that is for our fellow human beings with very weak defenses.
Which brings me to the question: how deadly is corona really? Do virologists and epidemiologists have a standard yardstick for that?
In the Netherlands we live with 17 million people. People are born every day, and people die every day. That is a natural process. If more people die than average, we speak of ‘over-death’. If fewer people die than average, we speak of ‘under-mortality’. In the Netherlands we had excess mortality in the months of March and April 2020. After that there was a period of under-mortality in our country for months.
We express the lethality of a virus with the IFR, the Infection Fatality Rate. That is the percentage of people who have been in contact with the virus who die from the virus. Corona has an estimated IFR of 0.5 percent or less. This can be compared to the IFR of a medium to severe flu.
Yes, corona is a new virus. But I want to make a case for moving from fear to trust. We count the brothers and sisters of the corona virus under our ‘medium winter flu’. Global panic is not necessary. People generally deal more rationally with the much more severe infections that you see in the tropics.
But in the US, a lot of people die from corona, right?
That’s right. In areas with a high mortality, it is striking that the socially deprived part of the population in particular is dying. This part of the population has an increased risk of a serious course of the disease, such as obesity and diabetes. Bad food, bad air, bad housing, bad (clean) water supplies all contribute directly or indirectly to a weakened immune system.
At the moment there is a lot of fuss about mouth masks in schools. What is your opinion about that?
Mouth masks may be of some help in preventing the virus from passing on to others if you have COVID-19 disease. In schools, however, the advantages seem smaller than the disadvantages: risk of breathlessness, concentration problems, headaches and possibly brain damage.
How do you think corona will continue in the coming months and years?
It is expected that we will have an increased risk of aerosols in the months of November to April. If we protect the vulnerable in society well, and if we ventilate well, the second wave will not be as intense as the first wave. After all, many people have already become acquainted with the virus. Also in the future, corona will keep coming back in the winter months. But it never has to be as fierce as last spring, when the virus was completely new to everyone.
You have devoted your life to studying infectious disease management. What do you notice worldwide in the approach to the corona virus?
Cutting back on care and slimming down the hospital bed stock has contributed significantly to the fear and panic measures to avoid being overrun by the volume of patients. Unfortunately, this does not only apply to Amsterdam East and the Netherlands.
Because the benefits of the cuts are often not evenly distributed, a large part of the world’s population has unfortunately become even more vulnerable to following a healthy lifestyle.
As far as the approach is concerned, I think that a study of the older literature and targeted research based on this can contribute to an effective policy. A policy devoid of fear, panic and the need to sacrifice personal freedoms.
Ivermectin studies
Prof. Thomas Borody has been using an Ivermectin-based tritherapy for treating Covid-19, and his results have been so successful that he’s on record saying “We Know it’s Curable; It’s Easier than Treating the Flu”.
Here are some recent studies (peer-reviewed and otherwise) regarding this.
- The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro
- Un estudio demuestra la respuesta antiviral de la ivermectina en pacientes con COVID-19
- Use of Ivermectin Is Associated With Lower Mortality in Hospitalized Patients With Coronavirus Disease 2019: The ICON Study
- Controlled randomized clinical trial on using Ivermectin with Doxycycline for treating COVID-19 patients in Baghdad, Iraq
Also, a two-parts interview with the prof.
The utter unreliability of PCR testing
I’ve written already on why there is abundant reason not to trust PCRs for diagnosis of the pandemic status of SARS-CoV-2. I’ve added that over-reliance on these methods can easily lead to psuedo-epidemics.
This time I want to present you with other factual sources on PCR.
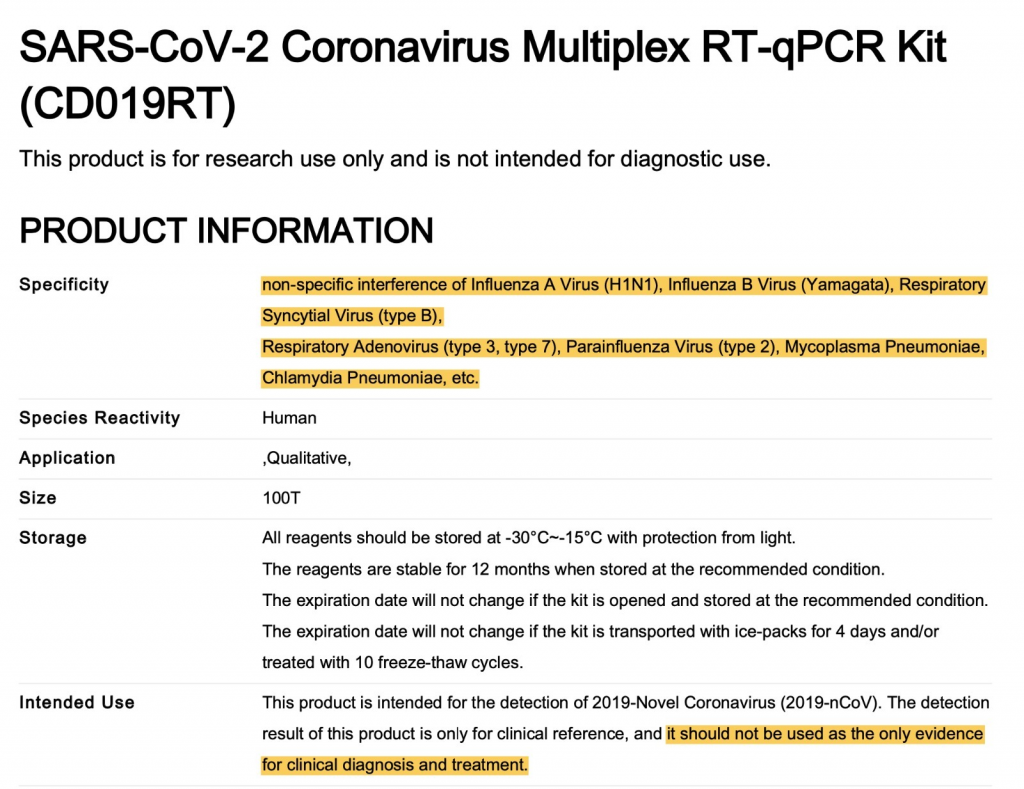
First, the picture above shows you part of a data sheet of a PCR kit for SARS-CoV-2. Notice the highlights:
- the test can suffer interference from a host of other common seasonal viruses
- the test should not be used as a sole evidence for clinical diagnosis and treatment
Second, article in the British Medical Journal clearly states:
RT-PCR tests can detect viral SARS-CoV-2 RNA in the upper respiratory tract for a mean of 17 days; however, detection of viral RNA does not necessarily equate to infectiousness, and viral culture from PCR positive upper respiratory tract samples has been rarely positive beyond nine days of illness.
Third, the Oxford Centre for Evidence Based Medicine’s article clearly explains that testing positive to PCR does not equate to infection:
A PCR test might find the virus it was looking for. This results in a PCR positive, but a crucial question remains: is this virus active, i.e. infectious, or virulent? The PCR alone cannot answer this question. The CEBM explains why culturing the virus is needed to answer this question:
“In viral culture, viruses are injected in the laboratory cell lines to see if they cause cell damage and death, thus releasing a whole set of new viruses that can go on to infect other cells.”
H1N1: the pandemic that wasn’t
Original article on Forbes. Copying as Forbes has been deleting its old articles that give support to the idea that WHO is faking this pandemic, too.
Mar 11, 2010,12:00pm EST, Henry I. Miller
The H1N1 swine flu outbreak appears to have ended less like the rogue wild boar that United Nations bureaucrats predicted and more like roasted pork tenderloin with apples and sage. From the beginning the World Health Organization’s actions have ranged from the dubious to the flagrantly incompetent.
Last June the WHO boosted the pandemic alert to the highest level, Phase 6. That meant that, according to the WHO, a pandemic was under way–the first time in 41 years that the organization had made such a declaration. But the WHO must have been suffering from four decades of amnesia because ordinary seasonal flu, which sweeps the world annually–and which is far more lethal than the currently circulating low-virulence H1N1 swine flu–certainly meets the organization’s definition of a pandemic: infections over a wide geographic area that affect a large proportion of the population.
Ironically, one might even consider the emergence of the H1N1 flu during the past year a net public health benefit, since it appears to have suppressed, or at least supplanted, the far more virulent and lethal seasonal flu strains. During the second week of January, 3.7% of Americans tested positive for the seasonal flu, compared with 11.5% during the same week last year. The death toll in the U.S. from H1N1 is estimated by the Centers for Disease Control and Prevention to be around 3,900, while in an average year seasonal flu kills about 36,000.
The WHO’s April 2009 decision to raise the pandemic flu threat to the penultimate level, Phase 5, “Pandemic Imminent,” was unwarranted and far outpaced the data accumulated. Even worse was the June declaration that a pandemic was under way, which exposed the WHO’s flawed fundamental paradigm. A warning system based solely on how widely a virus has spread, but that does not consider the nature, severity and impact of the illness it causes, is prone to false positives; it would classify not only seasonal flu but also the frequent but largely inconsequential outbreaks of virus-caused colds and gastroenteritis as “pandemics.” WHO has never offered any explanation for why these examples that seem to fit its definition of a pandemic do not meet its criteria.
False alarms make the “pandemic under way” designation almost meaningless, and they diminish its usefulness, which, in turn, has important consequences. As Dr. Jack Fisher, a professor of surgery at the University of California, San Diego, School of Medicine, observed, “Keep crying ‘wolf,’ and WHO can expect lower than customary compliance with flu vaccine advisories next fall.” Not only next fall, but also at some future time when we encounter a genuinely dangerous new pathogen such as a strain of H5N1 avian flu (which in its present form boasts a mortality rate more than 100 fold higher than the H1N1 swine flu) that is easily transmissible between humans.
The U.N.’s false alarms have had more immediate, negative effects. Matthew Hingerty, managing director of Australia’s Tourism Export Council, lamented that the country lost thousands of tourists because of the WHO’s pandemic declaration. Egyptian public health authorities overreacted and summarily ordered the slaughter of all the pigs in the country. In addition to the devastating economic losses, garbage filled the streets of Cairo and the numbers of rodents rose to fearsome levels because the pigs were no longer available to consume much of the garbage produced in the city. The U.N. indicted by the Law of Unintended Consequences.
The publicity and resulting panic surrounding the WHO’s announcement of Phase 5 and 6 alerts–especially since the vaccine was not widely available until December–also brought out the fraudulent peddling of all sorts of ineffective and possibly dangerous protective gear and nostrums, including gloves, masks, dietary supplements, shampoo, a nasal sanitizer and a spray that supposedly coats the hands with a layer of anti-microbial “ionic silver.”
For all these reasons, the declaration of a pandemic cannot be a prognostication but rather should be a real-time snapshot, and it must only be made when science and common sense support it.
WHO’s performance has been widely criticized. Most flu experts believe that the WHO’s actions were overly alarmist and precipitous and the Parliamentary Assembly of the Council of Europe announced that it plans to debate “false pandemics, a threat to health.”
And yet WHO officials continue to defend their actions. In a Jan. 14 conference call with reporters, Keiji Fukuda, special adviser to the WHO’s director general for pandemic flu, remonstrated that the organization had not overplayed the dangers but “prepared for the worst and hoped for the best.” Other communications were more strident. “The world is going through a real pandemic. The description of it as a fake is wrong and irresponsible,” the WHO said on Jan. 25. A particularly problematic statement came from WHO spokesman Greg Hartl, who said, “We cannot control how people react to” WHO announcements concerning pandemics. He would benefit from tutoring in risk communication.
The WHO’s dubious decisions demonstrate that its officials are too rigid or too incompetent (or both) to make needed adjustments in the pandemic warning system–deficiencies we have come to expect from an organization that is scientifically challenged, self-important and unaccountable. The WHO may be able to perform and report worldwide surveillance–i.e., count numbers of cases and fatalities–but its policy role should be drastically limited.
U.N. bureaucrats pose as authorities on all manner of products, public policy and human activities, from desertification and biodiversity to the regulation of chemicals, uses of the ocean and the testing of genetically engineered plants. However, the U.N.’s regulatory policies, requirements and standards often defy scientific consensus and common sense. Its officials are no friends of commerce, public health or environmental protection. The result is a more precarious, more dangerous and less resilient world. When it comes to pestilence, the U.N. may be the greatest plague of all.
Henry I. Miller, a physician, molecular biologist and former flu researcher, is a fellow at Stanford University’s Hoover Institution and at the Competitive Enterprise Institute. He was an official at the National Institutes of Health and Food & Drug Administration.
Pseudo-epidemics
Yes, you read it. Pseudo-epidemics. They are a real thing.
Though I am scientist by training, I am not a medical scientist or anything closely related. But I remain a scientist. The scientific method that underpins all the sciences doesn’t change.
That’s what allowed to have a critical eye on all this pandemic business.
Now, all the recent posts on this blog are there to point out one simple thing: the Covid-19 pandemic has ended in May. What we’re seeing now is what many scientists and medical doctors are calling a casedemic.
In short, due to pre-existing T-cell immunity and the now endemic nature of the virus, the over-reliance on PCR testing is causing a overwhelming high number of false positives. These false positives are what they call asymptomatic people. Unlike what the people in the media tell you, the reality about these people is that they are not actually sick.
A few days ago I found out that there’s an established term to refer to what’s happening right now with SARS-CoV-2. It’s called a pseudo-epidemic.
A sample of articles that talk about this phenomenon:
- Curbing false positives and pseudo-epidemics: “Pseudo-epidemics” may be on the rise because of an “over-reliance” on molecular diagnostic tests.
- False alarms and pseudo-epidemics: the limitations of observational epidemiology
- Pseudo-epidemics: Why COVID-19 is guaranteed to never end
From the latter I quote:
Given current definitions COVID-19 will never end. People will be dying of it forever, even if the virus disappears completely. Worse still, the system is locked in a series of feedback loops — if something causes test numbers to rise then so will case numbers, which in turn will cause a further increase in testing, causing the rise to continue, triggering local lockdowns and pointless evidence free rituals, until people get depressed and stop trying to do things causing numbers being tested to fall again.
A medic’s case against another lockdown
If lockdowns were a prescription drug for Covid-19 treatment, the FDA would never have approved it. The seminal Imperial College London paper and other mathematical models like it were used to justify their use, but clinicians would never prescribe a drug or propose a surgery based on such modelling. The now well-publicised failure of these models to accurately predict Covid-19 outcomes proves the rule.
In medical science, we rely on epidemiologists to take all the available data from all the countries and perform statistical analyses to correct for as many different variables as possible.
This has now been done for lockdowns. In August, the Lancet published an analysis of data from 50 countries. The researchers found that full lockdowns were ‘not associated’ with decreased mortality from Covid-19. These are hard outcome data; reality cannot be waved away with theories or projections.
https://www.spectator.co.uk/article/a-medic-s-case-against-another-lockdown
Covid-19: Do many people have pre-existing immunity?
I have already talked about the mounting evidence supporting widespread T-cell immunity against SARS-CoV-2 (Covid-19).
This study on the British Medical Journal (Covid-19: Do many people have pre-existing immunity?) is interesting because it’s one of the few places where a similar situation from 2009 is recalled. In fact, in 2009 we experienced a casedemic with H1N1, that is, a growing number of cases which however did not lead to an actual high mortality rate. I quote:
Swine flu déjà vu
In late 2009, months after the World Health Organization declared the H1N1 “swine flu” virus to be a global pandemic, Alessandro Sette was part of a team working to explain why the so called “novel” virus did not seem to be causing more severe infections than seasonal flu.12
Their answer was pre-existing immunological responses in the adult population: B cells and, in particular, T cells, which “are known to blunt disease severity.”12 Other studies came to the same conclusion: people with pre-existing reactive T cells had less severe H1N1 disease.1314 In addition, a study carried out during the 2009 outbreak by the US Centers for Disease Control and Prevention reported that 33% of people over 60 years old had cross reactive antibodies to the 2009 H1N1 virus, leading the CDC to conclude that “some degree of pre-existing immunity” to the new H1N1 strains existed, especially among adults over age 60.15
The data forced a change in views at WHO and CDC, from an assumption before 2009 that most people “will have no immunity to the pandemic virus”16 to one that acknowledged that “the vulnerability of a population to a pandemic virus is related in part to the level of pre-existing immunity to the virus.”17 But by 2020 it seems that lesson had been forgotten.
Structural stability of SARS-CoV-2 3CLpro and identification of quercetin as an inhibitor by experimental screening – ScienceDirect
Structural stability of SARS-CoV-2 3CLpro and identification of quercetin as an inhibitor by experimental screening – ScienceDirect
— Read on www.sciencedirect.com/science/article/pii/S0141813020339970
This is on top of Quercetin also being a Zinc ionophore, which helps increasing the amount of intracellular elemental zinc, which in turns inhibits replication of RNA viruses.